Overweight and obesity are a clear threat to public health in our times. Their prevalence has been growing and continues to do so, in recent years. In addition, many associated diseases and complications make this formidable problem even more difficult. And among them, non-alcoholic fatty liver disease stands out.
As common as it is underdiagnosed
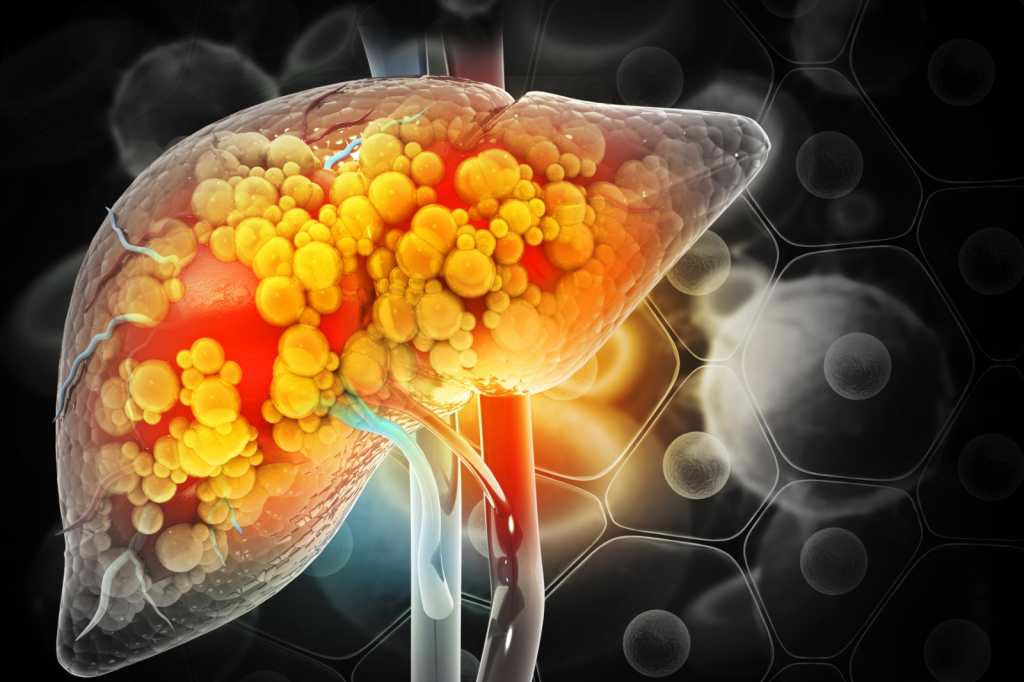
We are referring to the most common chronic liver disease in Western societies, affecting between 20 and 30% of the adult population. It is characterized by an excessive accumulation of fats inside the liver cells, which causes alterations in liver function.
The main problem is that it is usually not diagnosed, since the clinical assessment focuses on the underlying obesity, without going any further.
It has been observed that around 30% of patients with steatosis, without specific treatment or follow-up due to poor diagnosis, progress to an inflammatory process. And of these, around 20-25% end up developing cirrhosis after ten years.
Furthermore, among patients with cirrhosis, about 10% end up with hepatocellular carcinoma, i.e. liver cancer, after five years. Hence the importance of detecting the disease in time and treating it so that it does not progress to more advanced stages.
Furthermore, it could be an additional risk factor for cardiovascular disease, chronic kidney disease, endocrinopathies (including diabetes mellitus and adipose tissue dysfunction), and osteoporosis.
Although fatty liver has the additional problem of not presenting well-defined signs or symptoms, it is known that those affected may experience chronic fatigue, pain in the upper right part of the abdomen, and a slight increase in transaminases.
The only treatment: healthy diet and exercise
Currently, there are no specific pharmacological treatments for fatty liver disease, so therapeutic approaches focus on lifestyle modifications, aimed primarily at preventing associated risk factors. These changes consist of following nutritional guidelines based on the Mediterranean diet and doing regular physical exercise.
The Mediterranean diet is characterized by a high intake of vegetables, legumes, cereals, olive oil, nuts, fish, and dairy products, with little meat and moderate consumption of wine.
This traditional Mediterranean dietary pattern has been shown to have heart-healthy properties, helping to prevent diabetes and fatty liver disease, as well as reducing overweight and obesity. For all these reasons, it should be encouraged in the face of the increasing consumption of processed and unhealthy foods.
Secondly, staying active daily is very important for good health. It is advisable to reduce sedentary periods of more than two hours and, whenever possible, move around actively (walking or cycling).
On the other hand, if we follow the recommendations to do physical exercise regularly, we must take into account that each person, depending on their physical condition, will be able to carry out a specific activity adapted to their abilities. For example, for people who are overweight or obese, it is most advisable to, at least, walk every day, trying to reach ten thousand steps a day, and to carry out some type of additional personalized physical activity of about 30 minutes two or three days a week.
What results can be achieved?
Our Nutrition and Oxidative Stress Research Group (NUCOX) has conducted a study to find out the effects of diet and physical activity on fatty liver disease.
After carrying out a nutritional intervention and promoting physical exercise in patients aged between 40 and 60 living in the Balearic Islands, we were able to observe how the intrahepatic fat content, measured by nuclear magnetic resonance, decreased significantly. This implies a reduction in fatty liver disease which, in some cases, even resulted in a reversal of the condition.

In addition, participants who showed an improvement in liver fat content lost weight and experienced a decrease in triglyceride and transaminase levels. Transaminases are enzymes that, if present in the blood, indicate the presence of liver damage. We also linked physical activity with an improvement in fatty liver and aerobic capacity. Patients with positive results showed better physical condition and were less tired.
Patients who adhered most to the Mediterranean diet experienced the greatest improvement in their fatty liver disease and lost the greatest amount of fat. Finally, after the intervention, we observed an improvement in the biomarkers of oxidative stress and inflammation, which indicates a better functioning of the metabolism.
In conclusion
Non-alcoholic fatty liver disease is clearly on the rise and is directly linked to the increase in overweight rates. The lack of specific treatment and its relationship with other cardiometabolic diseases make it necessary to focus on preventing it through a healthy lifestyle. In this sense, diet and exercise can reduce intrahepatic fat content, enhance aerobic capacity and physical condition, and produce an improvement in the oxidative and pro-inflammatory state.























+ There are no comments
Add yours